How the 2027 Respiratory Therapy Exam Is Structured
Instead of the old two-exam process (TMC followed by the CSE), the 2027 respiratory therapy exam is now one unified exam that contains two types of multiple-choice questions:
1. Breadth-Focused Questions (General RT Knowledge)
These questions assess wide-ranging foundational knowledge across the respiratory care curriculum—such as patient data, oxygen therapy, ventilator basics, pharmacology, airway management, and infection control.
Think of this portion as your general RT competency check, similar to the old TMC-style knowledge base, but updated and modernized.
2. Depth-Focused Questions (Clinical Judgment & Decision-Making)
These questions go beyond recall. They require you to analyze patient information, interpret data, anticipate problems, and choose the safest evidence-based intervention.
They mirror real clinical decision-making by requiring the student to:
- identify relevant patient cues
- interpret ABGs, trends, or alarms
- prioritize safe interventions
- determine when to escalate care
- adjust therapy based on the patient’s response
These depth questions replace the old CSE-style scenarios but do so in a cleaner, multiple-choice format—no more branching simulations.
Why This Matters
Instead of preparing for two separate exams, candidates now prepare for one exam containing general knowledge questions and clinical judgment questions.
This structure aligns more closely with real practice: RTs must know the content and apply it safely at the bedside.ents can prepare.
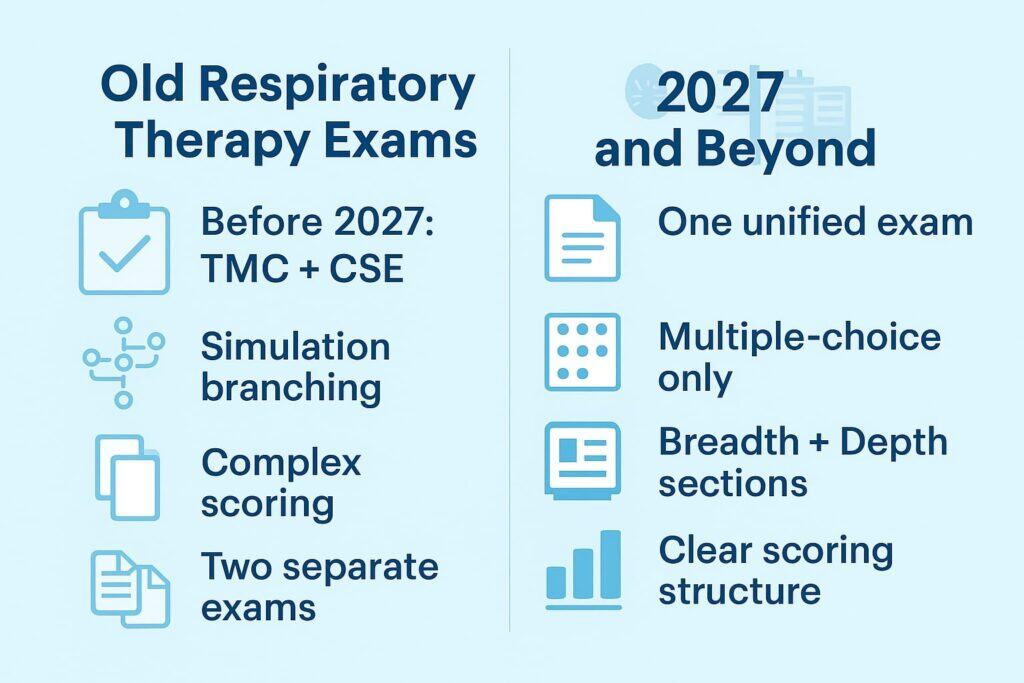
Why the NBRC Removed Simulations
The old CSE had branching clinical pathways that often confused students. The NBRC redesigned the exam to:
- standardize scoring
- remove subjective branching paths
- focus on reproducible decision-making
- improve test reliability
- align with modern exam design used in other national boards
- emphasize real-life reasoning instead of “guess the pathway” logic
The result is a more transparent, consistent, and clinically focused exam.
What “Depth” MCQs Actually Are
Depth items are not ordinary multiple-choice questions. They are scenario-based, layered MCQs that require the candidate to:
- analyze patient cues
- identify key vs. irrelevant findings
- determine clinical priorities
- anticipate complications
- choose the best action—not just a correct one
- integrate ethics, safety, culture, and communication into decisions
A depth item feels like a condensed clinical scenario:
You get a chunk of patient information → identify the priority → decide the safest next step.
No branching.
No scoring traps.
No simulations.
What Skills the 2027 Exam Prioritizes
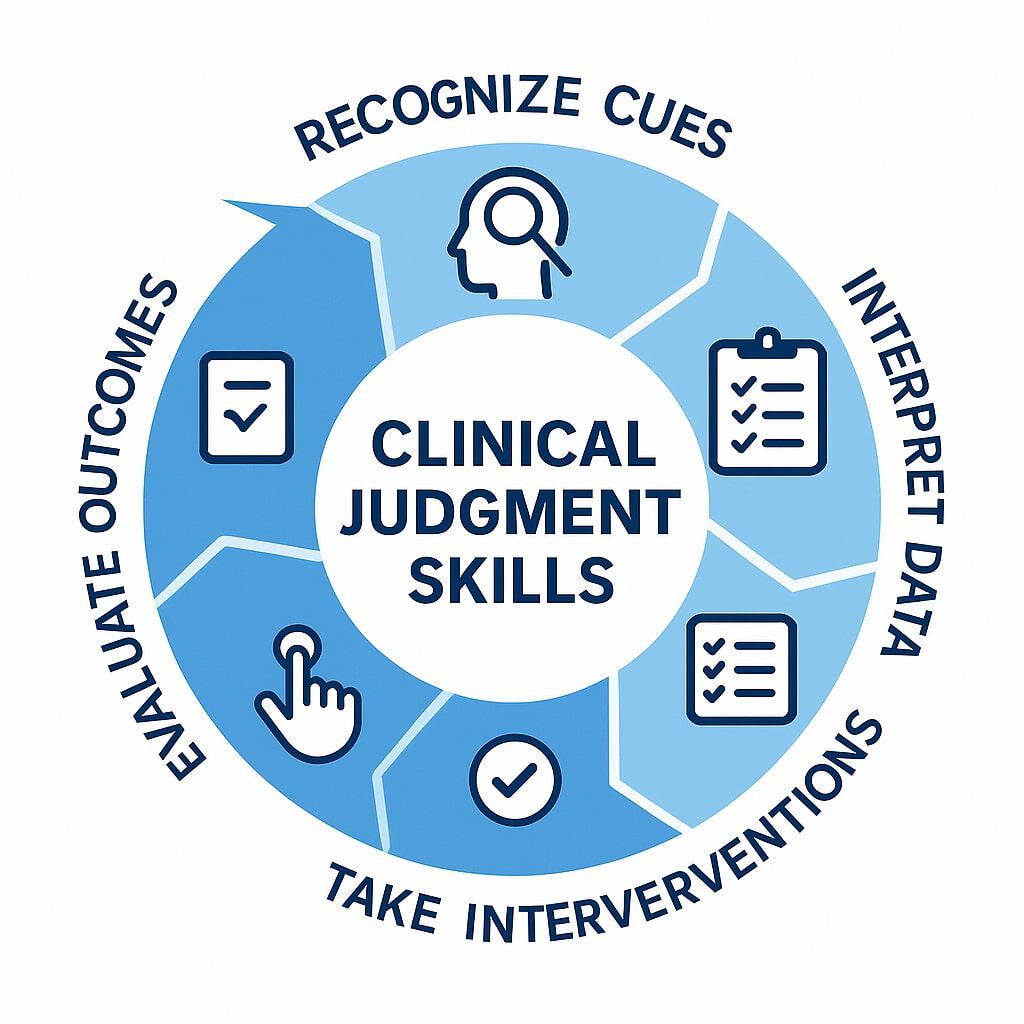
Depth questions target high-level cognitive skills essential for day-one safe practice:
1. Cue Recognition
Distinguishing important from unimportant data.
2. Trend Analysis
Interpreting changes in vitals, ventilator parameters, gas exchange, or patient status.
3. Prioritization
Choosing which action is the safest or most effective.
4. Anticipatory Thinking
Understanding what is likely to happen next if nothing changes.
5. Interprofessional Communication
Knowing how to escalate or clarify concerns.
6. Cultural & Trauma-Informed Considerations
Making patient-centered decisions shaped by beliefs, preferences, and trauma history.
7. Ethical Decision-Making
Choosing actions that balance autonomy, safety, and professional standards.
How Depth MCQs Are Structured
A typical question includes:
- Brief scenario (cues, vitals, labs, assessments)
- Clinical focus (e.g., oxygenation, communication, ethics, ventilation management)
- The prompt (“Which action is the MOST appropriate?”)
- Four answer choices (one best answer)
No partial credit.
No branching.
No multiselect.
Sample Scenario-Based MCQ (Aligned With 2027 Format)
A 65-year-old patient with COPD is receiving 2 L/min oxygen via nasal cannula. He is anxious, breathing rapidly, and repeatedly removes his oxygen. RR 32, HR 118, SpO₂ 86%, accessory muscle use present. He says, “I feel like I can’t breathe.”
Which action is the most appropriate?
A. Increase oxygen to 6 L/min and encourage slow breathing
B. Switch to a Venturi mask at 28% and coach pursed-lip breathing
C. Call for rapid response due to respiratory failure
D. Apply a nonrebreather mask at 15 L/min
Correct Answer: B
A Venturi mask improves oxygen delivery with controlled FiO₂ while minimizing risk of suppressing hypoxic drive. Coaching pursed-lip breathing reduces dynamic hyperinflation and anxiety.
Increasing nasal cannula to 6 L/min causes mucosal irritation and inconsistent FiO₂.
A rapid response is premature because the patient is unstable but responsive.
A nonrebreather is excessive and not indicated for stable COPD exacerbations.
This is the exact structure the NBRC is shifting toward.
How Students Should Prepare for the 2027 Exam
1. Practice reading long stems
Depth questions are data-heavy.
2. Prioritize safety first
The NBRC always rewards the safest action.
3. Use a structured decision-making method
Example:
- What cues matter?
- What condition is likely developing?
- What is the safest next step?
4. Strengthen pharmacology and interactions
Medication choices are more prominent in 2027.
5. Review ethics, communication, and cultural care
These are now tested explicitly.
6. Practice trend recognition
Especially ventilator changes, ABGs, and vital signs.
Why This Format May Help Students Pass
The new scenario-based multiple-choice format is actually more fair because:
- you aren’t penalized for mis-clicking a simulation path
- grading is standardized and objective
- every question gives you all the information you need
- candidates can focus on clinical reasoning, not navigating software
The 2027 exam reflects how real RTs think—interpreting cues, making safe decisions, and communicating effectively.

